Cortisol – The Stress Hormone: Significance, Diagnostics and Effects on Your Health
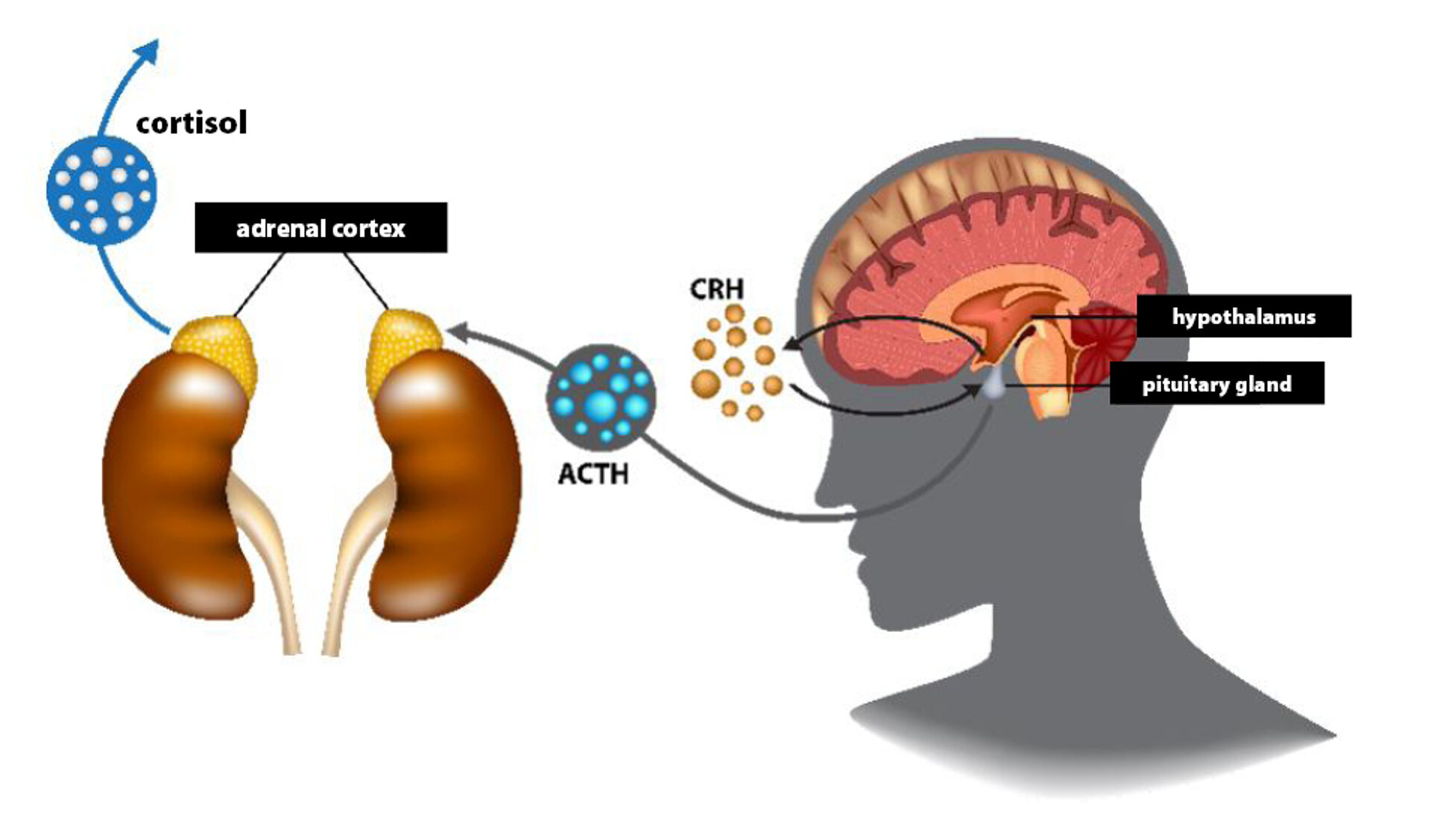
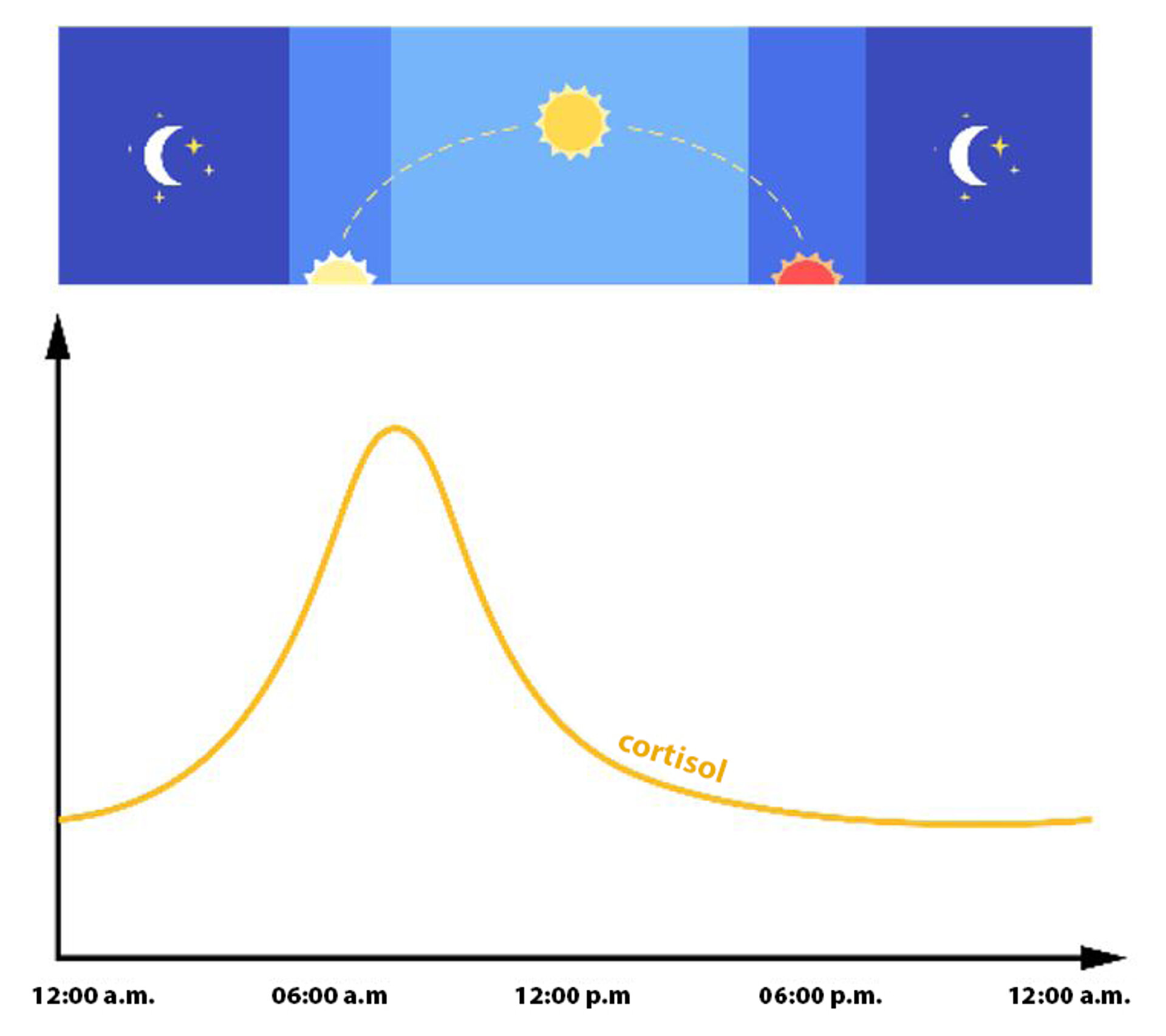
Glucocorticoids belong to the corticosteroids, a class of steroid hormones that are primarily produced in the adrenal cortex. Glucocorticoids play a central role in many critical biological processes such as growth, reproduction and metabolism, as well as in the regulation of immune and inflammatory responses. They also help maintain the homeostasis of the cardiovascular and central nervous systems. The most important endogenous glucocorticoid is cortisol (hydrocortisone), the production of which is controlled by a highly sensitive regulatory circuit known as the hypothalamic-pituitary-adrenal (HPA) axis (also referred to as the cortisol axis) (Fig. 2). Physiological cortisol production follows a circadian rhythm (Fig. 1). In preparation for the demands of the day, the hypothalamus releases increased amounts of corticotropin-releasing hormone (CRH) in the morning to provide glucose and energy. CRH in turn induces the secretion of adrenocorticotropic hormone (ACTH) from the pituitary gland. ACTH directly stimulates cortisol synthesis in the adrenal cortex, which results in cortisol levels peaking in the morning upon waking (CAR, Cortisol Awakening Response). Over the course of the day, cortisol levels gradually decline and reach a minimum around midnight.
Range of Cortisol Effects in the Body
Physiological Effects
Cortisol increases energy turnover by activating catecholaminergic stress hormones, while also raising body temperature and heightening alertness. Additionally, the uptake of glucose into peripheral tissues is inhibited. This inhibition of glucose uptake, together with the suppression of protein biosynthesis, results in elevated blood sugar levels. Acting on the cardiovascular system, cortisol helps regulate blood pressure and cardiac output according to demand. Cortisol also influences sleep, memory consolidation, mood and appetite regulation.
Summary of Effects:
- Suppression of the hypothalamic-pituitary-adrenal (HPA) axis
- Increase in energy metabolism and mobilisation of energy reserves
- Promotion of gluconeogenesis
- Increase in lipolysis
- Promotion of protein breakdown in muscles, bones and connective tissue
- Reduction of protein biosynthesis in lymphatic tissues
- Immunosuppressive action
- Control of inflammatory responses
Consequences of a Disturbed Cortisol Balance
Given the multitude of neuroendocrine interconnections of cortisol, an excess of cortisol can lead to metabolic disorders such as obesity, visceral fat distribution and elevated blood lipid levels, as well as diabetes, immune deficiencies and impaired infection and tumour defences. This is due to the suppression of the cellular immune response, alongside a relative enhancement of the humoral immune response. Impaired reactivity to endogenous glucocorticoids can result in depressive disorders or chronic fatigue syndrome.
Therapeutically, glucocorticoids act via this mechanism in inflammatory conditions, diseases associated with pathological immune activation (asthma, atherosclerosis, chronic inflammatory bowel disease) or autoimmune diseases (multiple sclerosis, rheumatoid arthritis). Therefore, they are frequently used as anti-symptomatic medication.
How Stress Affects Cortisol Levels
Irrespective of the circadian rhythm, physical or psychological stress stimuli cause a significant increase in cortisol levels at any time of day. In acute physical or emotional stress situations, cortisol release increases. In cases of chronic or traumatic stress, however, a decrease in cortisol secretion can also occur.
Acute Stress
The body responds to stress stimuli by mobilising energy reserves, increasing basal metabolic rate, accelerating circulation and breathing, improving blood flow to the muscles and enhancing alertness. At the same time, bodily functions not associated with fight-or-flight are inhibited, such as digestion, the immune system, sexual organs and pain perception. Reactions may occur faster, albeit with a higher error rate. These are normal physiological processes, which have no negative effects if adequate recovery occurs. They become detrimental when the number and intensity of stressors overwhelm physiological compensatory mechanisms. The coordinated activation of stimulating and inhibitory processes is crucial for maintaining the balance of these regulatory circuits and for quickly restoring normal conditions.
Chronic Stress
If the number, duration and intensity of stressors exceed the capacity of stress regulation circuits, the body enters a “permanent alarm” state, which can significantly impair health over time. Moreover, this becomes a self-reinforcing process: stress breeds stress. As a result, increasingly minor stimuli can trigger a stress response, which may eventually become chronic.
Stress-Induced Hypo- and Hypercortisolism
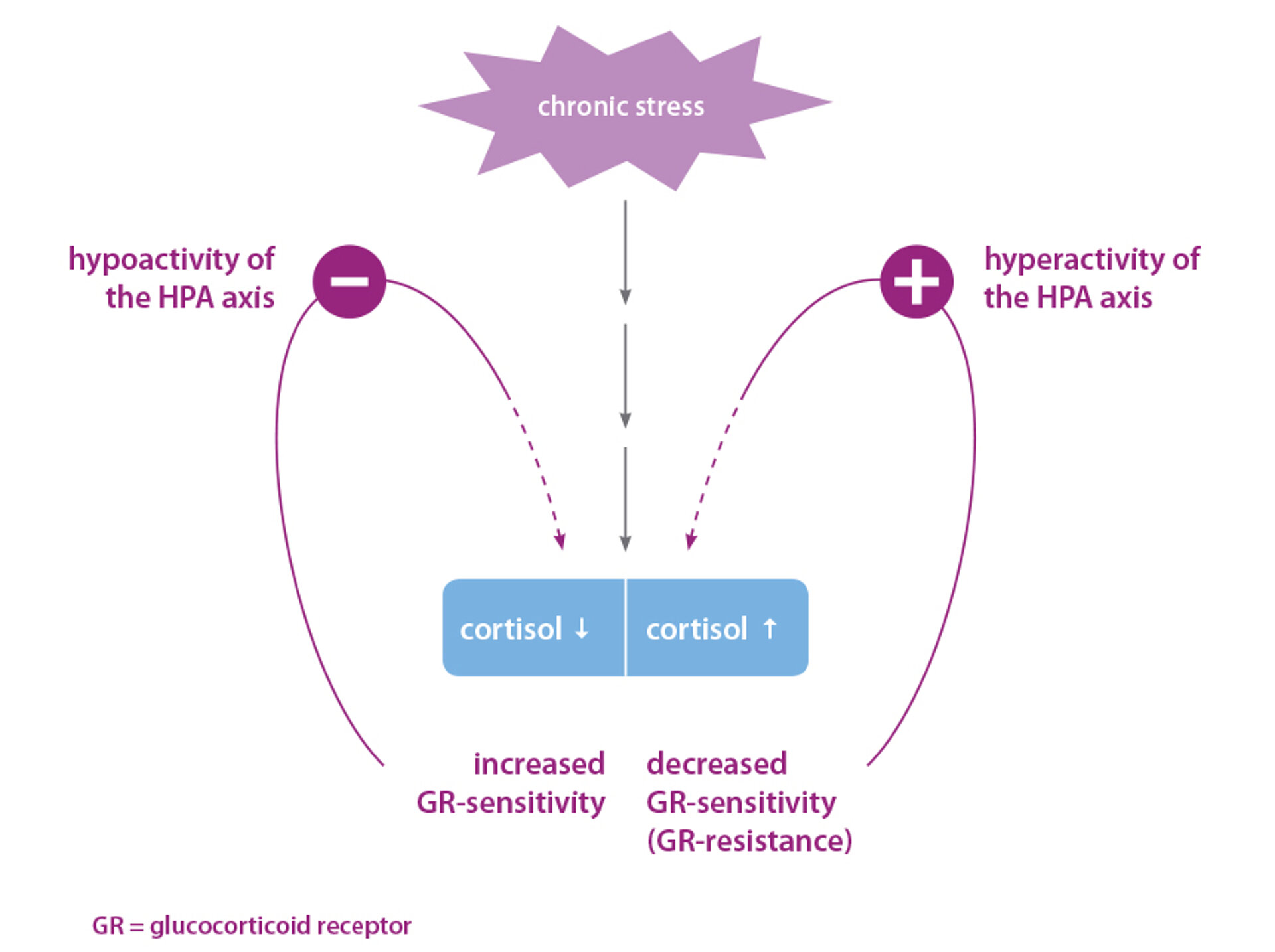
Until recently, stress-related illnesses were believed to be exclusively associated with elevated cortisol levels (hypercortisolism) due to activation of the HPA axis. However, newer research shows that a lack of cortisol (hypocortisolism) can also be clinically relevant (Fig. 3). In fact, 20-25% of individuals with chronic or traumatic stress develop relative hypocortisolism.
The causes may include CRH or ACTH deficiency, cortisol deficiency, or increased cortisol sensitivity in target cells. Chronic stress also disturbs the balance of other neurotransmitters and hormones. The imbalance in the neurotransmitter system leads to various health problems, notably fatigue, lack of drive, migraines and sleep disorders. Individuals with lower self-confidence and a tendency towards depression exhibit a pronounced, often persistent activation of the cortisol axis.
Cortisol and Immune Function
Chronically elevated cortisol levels suppress both specific and non-specific cellular immune defences. Cortisol inhibits the release of arachidonic acid as well as the formation of prostaglandins and leukotrienes, and blocks the synthesis of pro-inflammatory gene activators such as NF-κB, as well as the release of additional inflammatory mediators like interleukin (IL)-1 and IL-6. The possible consequences are increased susceptibility to infections and weakened early defence against cancer cells.
Cortisol and Brain Activity
Persistently high cortisol levels can trigger neurotoxic effects in the central nervous system (CNS), thereby promoting cerebral degenerative processes. Earlier studies have already shown a connection between chronic stress and the risk of developing neurodegenerative diseases such as Alzheimer’s disease. Elevated cortisol levels seem to accelerate the degeneration and death of neurons. This is associated with impaired memory function in otherwise healthy elderly men and women. Individuals exposed to high levels of stress had twice the risk of developing Alzheimer’s disease compared with those without significant stress exposure. Therefore, reducing high stress-induced cortisol levels is crucial for the recovery and regeneration of brain cells. This can be achieved through physical exercise and alternating relaxation and tension techniques, such as autogenic training and brain exercises.
Cortisol and DHEA
The counterpart of the stress hormone cortisol is the “vitality hormone” DHEA (dehydroepiandrosterone). This steroid hormone is produced in the adrenal cortex and plays a key role in the biosynthesis of sex hormones. Under physiological conditions, the release of DHEA and cortisol occurs synchronously – depending on CRH and ACTH secretion. With increasing age, DHEA production declines, while cortisol production remains constant. Consequently, the cortisol/DHEA ratio increases significantly with age. Patients who developed dementia in old age showed a significantly higher cortisol/DHEA ratio compared to cognitively healthy elderly individuals.
Numerous studies indicate that the cause of many age-related diseases is rooted in a decline in DHEA levels. For this reason, the cortisol-to-DHEA ratio is regarded as an indicator of the ageing process.
Taking DHEA supplements appears to increase individual “stress resistance” and protect against a range of age-related diseases. For example, higher DHEA levels are associated with increased bone density. Conversely, reduced DHEA levels are often observed in patients with an elevated risk of atherosclerosis and type 2 diabetes. Additionally, there is a negative correlation between DHEA levels and markers of chronic inflammatory activity.