Endocrinology
Precise Endocrine Diagnostics
Endocrinology deals not only with the function of hormones but also with their diagnosis and treatment. Diagnostics often include the assessment of hormone levels in the blood and saliva to enable a sound analysis of hormonal balance.
What are hormones?
Hormones are biochemical messengers produced by specific glands in the body. They are a central focus of endocrinology as they regulate vital bodily functions, including:
- Energy and water balance
- Reproduction
- Growth
- Emotions
- Sexual development
- Stress and anxiety responses
The Role of Hormones: Regulation of Vital Processes
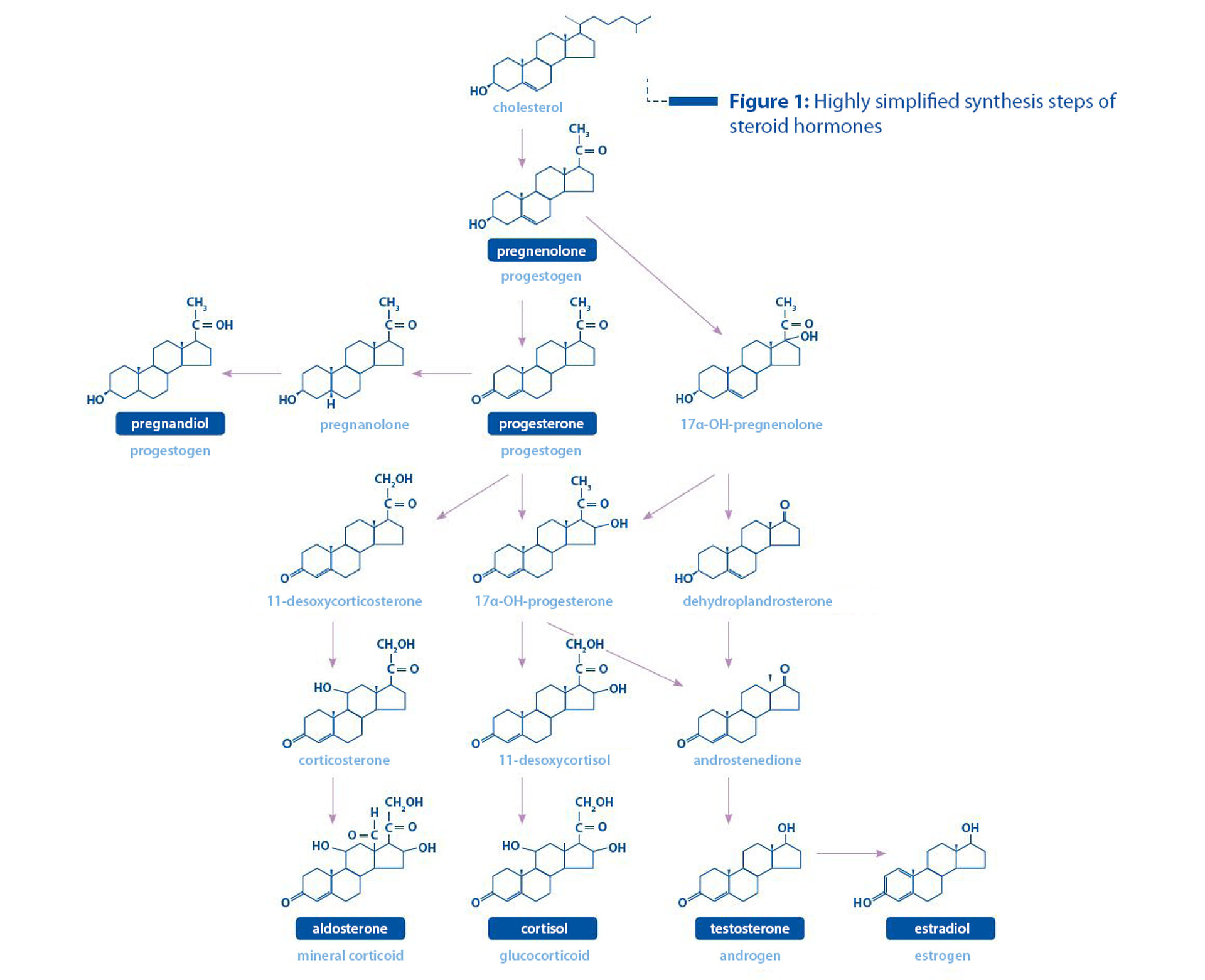
In endocrinology, hormones are often classified according to their chemical structure and function. These classifications help in understanding their diverse effects in the body. Steroid hormones, which are derived from cholesterol, are a key topic in endocrinology. Examples include sex hormones such as androgens, oestrogens, and progestogens, as well as corticosteroids produced by the adrenal cortex (see Figure 1).
Sex Hormones – A Central Focus of Endocrinology
Sex hormones are the ones responsible for the development and function of the reproductive organs, secondary sexual characteristics, sperm production, and the maintenance of the female cycle. They also influence sexual behaviour and reproduction.
Testosterone
Androgens are the collective term for male sex hormones, with testosterone being the most well-known. As an endocrine messenger, testosterone regulates various bodily functions. It ensures the development and function of the male reproductive organs, supports anabolic cell growth, and influences male physical characteristics such as body hair. Testosterone is mainly produced in the male gonads but also in smaller amounts by the male and female adrenal glands as well as by the female ovaries. In women, testosterone plays a key role in libido, muscle mass maintenance, and bone density. Imbalanced testosterone levels can disrupt the menstrual cycle and impair fertility.
Oestrogen
Oestrogens are a group of steroid hormones that perform numerous functions, especially in regulating the female reproductive system and secondary sexual characteristics. They are synthesised from cholesterol through several intermediate steps, which involve androgen precursors. The collective term oestrogens includes estradiol, estrone, and estriol. Oestrogens are primarily produced in the ovaries, with small amounts also formed in the adrenal glands. After menopause and in obese women, oestrogens are increasingly produced in fat and muscle cells.
Oestrogen deficiency naturally occurs during menopause but may also result from hormonal disorders, stress, poor nutrition, extreme physical activity, or medical treatments (e.g. chemotherapy).
Possible consequences of oestrogen deficiency:
- Menstrual disorders
- Sleep disturbances
- Hot flushes and night sweats
- Osteoporosis
- Dry skin/mucous membranes
- Mood swings
- Loss of libido
Oestrogen dominance (excess relative to progesterone) can result from obesity, stress, or menopause.
Common symptoms of oestrogen dominance:
- Psychological symptoms: depression, irritability, aggression, difficulty concentrating, restlessness, nervousness, anxiety, panic attacks
- Menstrual and cycle disorders (spotting, shortened cycles (polymenorrhoea))
- Sleep disturbances
- Increased body fat
Men also produce small amounts of oestrogen, which are important for bone density, heart health, sperm production, and cognitive function. In men, oestrogens are mainly formed through the conversion of testosterone by the enzyme aromatase in tissues such as the testes or fat cells.
Progesterone
Alongside oestrogens, progestogens are the second essential class of female sex hormones. The most relevant progestogens include the prohormone pregnenolone, progesterone, and its breakdown product pregnanediol. In women, progesterone is mainly produced in the ovaries – specifically the corpus luteum – during the second phase of the menstrual cycle. During pregnancy, it is produced by the placenta to maintain pregnancy (“pregnancy hormone”).
Physiological significance of progesterone:
- Initiation of the luteal phase
- Preparation and maintenance of pregnancy
- Bone stability
- Promotion of collagen production
- Sleep-inducing effect
- Counteracting mood swings
The main role of progesterone is to prepare the uterus for implantation and support of the fertilised egg and to protect the foetus during pregnancy. From around the fourth month of pregnancy, the placenta takes over progesterone production after the corpus luteum degenerates.
Benefits and Risks of Progesterone Therapy
Progesterone is considered a natural counterpart to oestrogens. Unlike oestrogens, progesterone replacement therapy is often seen as risk-free. However, current data suggest that even natural progesterone should be used cautiously. It can potentially promote tumour development, growth of microtumours, and metastasis formation. Therefore, as with any pharmacological treatment, even natural progesterone can have side effects.
The guiding principle of progesterone therapy is that treatment should be based on the patient’s symptoms. If there are no clear signs of progesterone deficiency, hormone therapy should be reconsidered even if lab results show low progesterone levels.
Although traditionally viewed as a "female" hormone, progesterone also has several important functions in men. It is a precursor in testosterone synthesis, helps maintain hormonal balance, supports the nervous system, reduces inflammation, and stabilises mood and sleep.
When Hormones Cause Problems – Menopause or Hormonal Imbalance?
Middle-aged women often report vague symptoms in medical consultations such as reduced libido, hot flushes, or irregular periods – symptoms frequently (and often incorrectly) attributed solely to menopause. These are among the most common challenges in endocrinology. Men in this phase of life may experience hair loss, weight gain, or fertility issues. Such symptoms are not always due to age-related hormonal decline but may result from hormonal imbalances. Hormonal balance is influenced by the activity of metabolising enzymes and is highly sensitive to lifestyle, environmental factors, and illness – all of which increase the risk of altered androgen or oestrogen activity and, subsequently, hormone-dependent cancers such as prostate, uterine, or breast cancer.
Cortisol – The Stress Hormone in Endocrinology
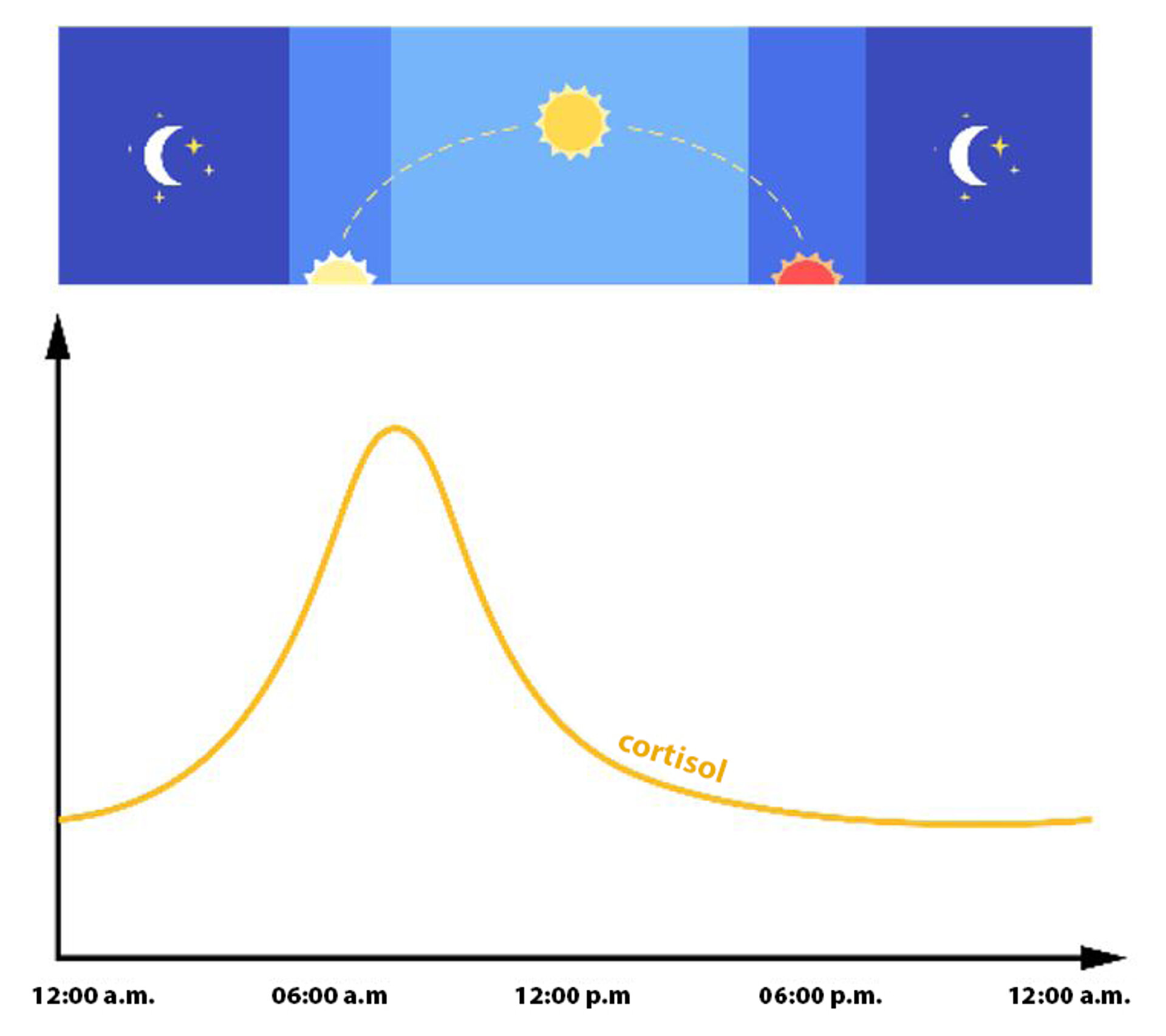
Glucocorticoids belong to the corticosteroids – a class of steroid hormones mainly produced in the adrenal cortex. The primary endogenous glucocorticoid is cortisol (hydrocortisone), which is released via the highly sensitive hypothalamic-pituitary-adrenal (HPA) axis. Cortisol is secreted in a circadian rhythm. It peaks in the early morning and reaches its lowest levels at midnight.
Regardless of this daily rhythm, physical or psychological stress can cause a significant increase in cortisol at any time. Alongside catecholamines, cortisol is the most important stress hormone and can rise 5- to 10-fold during stress.
Its main function is to provide energy by mobilising stored energy sources during acute or chronic stress.
The body responds to acute stress by increasing metabolism, circulation, respiration, blood flow to muscles, and alertness – while suppressing digestion, immunity, reproductive functions, and pain perception. These are normal physiological responses that typically have no negative consequences if followed by rest. However, in chronic stress, the stress axis remains overactive, which leads to persistently elevated night and morning cortisol levels. If prolonged, this disrupts the normal cortisol rhythm, which causes erratic fluctuations.
Disorders in glucocorticoid production can lead to pathological or life-threatening conditions such as hypercortisolism (Cushing’s syndrome) and hypocortisolism (Addison’s disease).
Hormone Diagnostics in Endocrinology – What, when, how, and where?
Endocrinology offers various diagnostic methods to assess hormones. Total steroid hormone levels (free and bound) can be measured in blood. Most are bound to transport proteins such as albumin, CBG (corticosteroid-binding globulin), and SHBG (sex hormone-binding globulin). However, only the free hormone fraction is biologically active. Saliva testing assesses this bioactive, free steroid fraction (especially cortisol) and is also used to monitor topical bioidentical hormone therapy (e.g. oestrogens or progesterone). Salivary steroids represent only 1-5% of the total blood hormone levels. Thus, saliva testing cannot assess total hormone synthesis, metabolism, or binding protein levels.
Because steroid concentrations in blood can be 100 times higher than in saliva, contamination of saliva samples with blood must be avoided. Only colourless saliva samples should be analysed.
Due to its reliability and ease of sample collection, salivary diagnostics is increasingly used in research and. Especially for cortisol rhythm analysis, it is now a standard tool in routine diagnostics.
Table: Diagnostic Recommendations for Free Steroid Hormones and Binding Proteins in Serum and Saliva
| Parameter | Diagnostic Material | Indication | Explanation |
| CBG* | Serum |
| High concentrations indicate an increased binding capacity for cortisol and progesterone and may also suggest reduced hormonal effectiveness. |
| Cortisol | Saliva |
| Free, bioactive cortisol in saliva allows for a quantitative estimation of active hormone levels in the blood and provides crucial information about the biologically effective cortisol concentration. |
| Testosterone & SHBG** | Serum |
| Free testosterone index, bioactive fraction of testosterone |
Oestradiol | Serum |
| Total oestradiol concentration: quantitative estimation of hormone levels in the blood (provides information about the biologically active oestradiol concentration) |
Oestradiol | Saliva |
| Unbound oestradiol: evidence of the therapeutic agent's absorption into the bloodstream and an increase in the bioactive hormone fraction ! Only the clinical symptoms determine the success of the therapy. |
| Progesterone | Serum |
| Total progesterone concentration: quantitative estimation of hormone levels in the blood (provides information about the biologically active progesterone concentration) |
| Progesterone | Saliva |
| Unbound progesterone: evidence of the therapeutic agent's absorption into the bloodstream and an increase in the bioactive hormone fraction ! Only the clinical symptoms determine the success of the therapy. |
| Albumin | Serum |
| Despite their low affinity, a significant proportion of hormones are bound to albumin. Markedly elevated or decreased albumin levels can therefore influence the biologically active fraction of steroids in the serum. |
* CBG = corticosteroid-binding globulin ** SHBG = sex hormone-binding globulin
Insulin – The Pancreatic Hormone
Insulin is produced in the pancreas and plays a key role in endocrinology and energy metabolism. It regulates blood glucose by facilitating the uptake of glucose into cells for energy or storage as glycogen. Dysfunction in insulin production or action leads to diabetes. Diabetes mellitus is a chronic metabolic disorder characterised by high blood glucose (hyperglycaemia). It occurs due to either absolute insulin deficiency (Type 1) or insulin resistance with relative insulin deficiency (Type 2).
Types of Diabetes Mellitus
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease, which causes the immune system to attack and destroy the insulin-producing beta cells in the pancreas. According to current scientific knowledge, the exact causes of type 1 diabetes are still not fully understood. However, various possible causes are being discussed. These focus mainly on genetic factors (family predisposition, autoimmune processes) and environmental factors (viral infections). Therefore, type 1 diabetes is considered a complex interplay of different factors that cause the immune system to attack and destroy the insulin-producing cells of the pancreas.
Type 1 diabetes usually begins in childhood or adolescence, though it can occur at any age. Treatment requires lifelong insulin therapy, regular blood glucose monitoring, and adjustments to various lifestyle factors such as diet and physical activity.
Type 2 Diabetes
Type 2 diabetes is a multifactorial condition caused by a combination of genetic and lifestyle factors (such as overweight and obesity, unhealthy diet, and lack of physical activity). In contrast to type 1 diabetes, where the immune system destroys the insulin-producing beta cells of the pancreas, type 2 diabetes is characterised by insulin resistance and a relative insulin deficiency. In insulin resistance, the body’s cells respond less sensitively to insulin. Although sufficient insulin may be present, it cannot effectively act on the cells, and glucose uptake into the cells is impaired. As a result, a relative insulin deficiency develops, which means that the pancreas cannot produce enough insulin to meet the body’s increased needs (i.e. the cells are resistant). The combination of insulin resistance and insufficient insulin production eventually leads to elevated blood glucose levels, which are characteristic of type 2 diabetes. Therefore, managing and preventing type 2 diabetes requires a comprehensive approach involving lifestyle changes and, if necessary, medication. The condition typically develops in adulthood but is increasingly seen in younger people as well. Treatment options range from lifestyle modification (diet and exercise) to oral antidiabetic medications and, in more advanced stages, insulin therapy.
A healthy diet, regular physical activity, and maintaining a healthy body weight can significantly reduce the risk of developing type 2 diabetes.
Special Case: Gestational Diabetes
Gestational diabetes occurs when blood sugar levels rise during pregnancy. In many cases, blood glucose levels can be normalised during pregnancy through sufficient physical activity and a balanced diet. If this is not successful, insulin injections may be required. Usually, blood glucose levels return to normal after childbirth. Nevertheless, continued monitoring of blood sugar levels is recommended.
Women who experience gestational diabetes have an increased risk of developing type 2 diabetes later in life.