Type 2 Diabetes: Diagnostics and Modern Approaches to Preventive Healthcare
Currently, more than 7% of all adult German citizens are receiving medical treatment for type 2 diabetes. In addition to genetic predisposition, diet and lifestyle play a decisive role in the development of type 2 diabetes. In particular, chronic excessive sugar consumption (sweets, processed foods, sugary drinks), smoking, alcohol, lack of exercise, and over- or malnutrition are risk factors for insulin resistance, which leads to diabetes in 5 to 10% of those affected. Early diagnosis of prediabetic stages makes it possible to prevent disease progression and potential (late) complications, often even without medication.
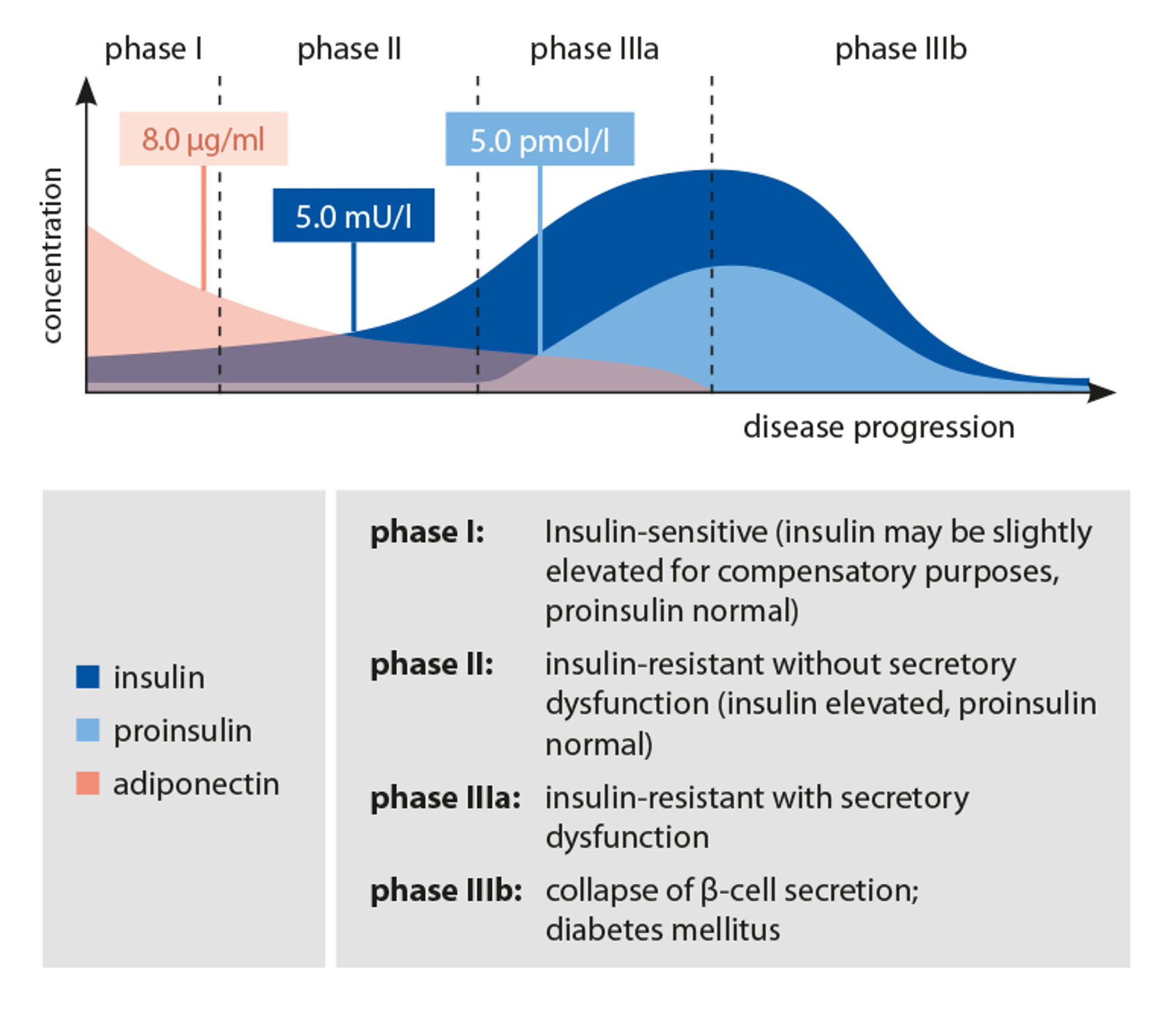
The causes of diabetes progression lie in a worsening insulin resistance, an (additional) dysfunction of the pancreatic β-cells, and chronic inflammatory processes within the blood vessel walls. Insulin resistance serves as a crucial link between type 2 diabetes and cardiovascular complications. Newly diagnosed diabetes patients typically present with multiple accompanying risk factors of the metabolic syndrome, such as obesity, arterial hypertension, and dyslipidaemia.
In addition to blood glucose and HbA1c parameters, biomarkers such as adiponectin, insulin, proinsulin, and leptin, as well as inflammatory markers (CRP, PAI-1, TNF-α, IL-6, and IL-8), are increasingly used to assess insulin resistance and pancreatic β-cell function.
The 3 Stages of Prediabetes
The prediabetic phase is divided into three stages with gradual transitions:
Stage 1: Early Stage of Insulin Resistance
The early stage of insulin resistance is usually characterised by adequate, compensatory β-cell activity in the pancreas. Fasting glucose levels are normal in this stage, as are fasting insulin levels.
At this stage, insulin sensitivity can often be improved through dietary measures and lifestyle changes alone, thereby preventing progression to stage 2.
Stage 2: Stage of Rising Insulin Levels
Stage 2 is characterised by impaired glucose tolerance. In most cases, the compensatory increase in insulin secretion can prevent hyperglycaemia. However, if early signs of impaired β-cell function are already present, hyperglycaemia will follow in the absence of therapeutic intervention.
In stage 2, dietary measures and lifestyle changes combined with micronutrient supplementation – and, in some cases, the use of oral antidiabetics such as glitazones – can improve insulin sensitivity. Appropriate glucose regulation can be restored with these measures, thereby preventing progression to stage 3.
Stage 3: β-Cell Dysfunction
In stage 3, type 2 diabetes mellitus develops due to progressive β-cell dysfunction in the pancreas. Glucose and HbA1c levels are significantly elevated, while fasting insulin levels may be normal or increased, depending on β-cell function.
At this stage, in addition to dietary measures, lifestyle changes, and micronutrient supplementation, targeted pharmacological therapy is necessary.
Metabolic Markers of Prediabetes
Adiponectin
Adiponectin is a peptide hormone produced exclusively in fat cells. Together with leptin, insulin, and other hormones, it regulates appetite. It increases insulin sensitivity in fat cells, the liver, and skeletal muscles, and is therefore involved in regulating glucose metabolism.
Low adiponectin levels are observed in patients with obesity, insulin resistance, and type 2 diabetes. There is a negative correlation between this hormone and the occurrence of cardiovascular risk factors such as hypertension, hypertriglyceridaemia, low HDL cholesterol levels, and inflammatory markers like C-reactive protein (CRP) and the fibrinolysis marker PAI-1. Studies have shown that consistent calorie reduction, weight loss, and regular physical activity can increase adiponectin levels.
Insulin
Insulin is a hormone produced by the pancreatic β-cells in response to glucose stimulation. Following insulin release, liver, fat, and muscle cells absorb glucose from the blood. Furthermore, insulin is crucial for storing glucose as glycogen in the liver; it suppresses hepatic glucose synthesis, and inhibits fat breakdown. High insulin levels are associated with an increased risk of diabetes.
Proinsulin
Proinsulin, the precursor of insulin, is produced and stored in the pancreatic β-cells. When required, it is converted into insulin through enzymatic cleavage of the C-peptide. Active insulin is then released into the bloodstream. In healthy individuals, only small amounts of intact proinsulin are found in the blood.
Leptin
Leptin is a protein hormone produced primarily in adipocytes, but also in smaller amounts in the gastric fundus, skeletal muscle, liver, and placenta. It plays a key role in regulating body weight. Loss of leptin function, possibly due to impaired leptin transport, leads to insulin resistance. Elevated leptin levels are associated with pancreatic β-cell dysfunction and an increased risk of type 2 diabetes mellitus.
Haemoglobin A1c (HbA1c)
Haemoglobin A1c refers to the percentage of glycated haemoglobins relative to total haemoglobin. It is a measure of the average blood glucose levels over the past 6-12 weeks, which corresponds roughly to the lifespan of a red blood cell. It is important to note that significant fluctuations in blood glucose levels can sometimes give a false-normal HbA1c value. The determination glycated proteins like HbA1c is used for monitoring metabolic control in diabetics. In healthy individuals, the proportion of glycated haemoglobins ranges between 4% and 6%. HbA1c values above 7% indicate diabetes mellitus.
The risk of cardiovascular disease is closely linked to HbA1c levels: an increase of 1% in HbA1c raises the risk of cardiovascular events or mortality by 20-30%.
HOMA-IR (Insulin Resistance)
HOMA-IR stands for “Homeostatic Model Assessment-Insulin Resistance” and is used to detect insulin resistance. In diabetes mellitus, a false-normal HOMA-IR index may be calculated if impaired β-cell function causes increased proinsulin secretion in the fasting state. A high HOMA-IR index can precede the onset of diabetes mellitus by several years.
To assess the risk of developing type 1 diabetes, antibodies in the blood can be measured: GAB II antibodies (glutamate decarboxylase antibodies), IA2 antibodies (tyrosine phosphatase antibodies), ICA (islet cell antibodies), and insulin autoantibodies.