Chronic Inflammatory Bowel Diseases
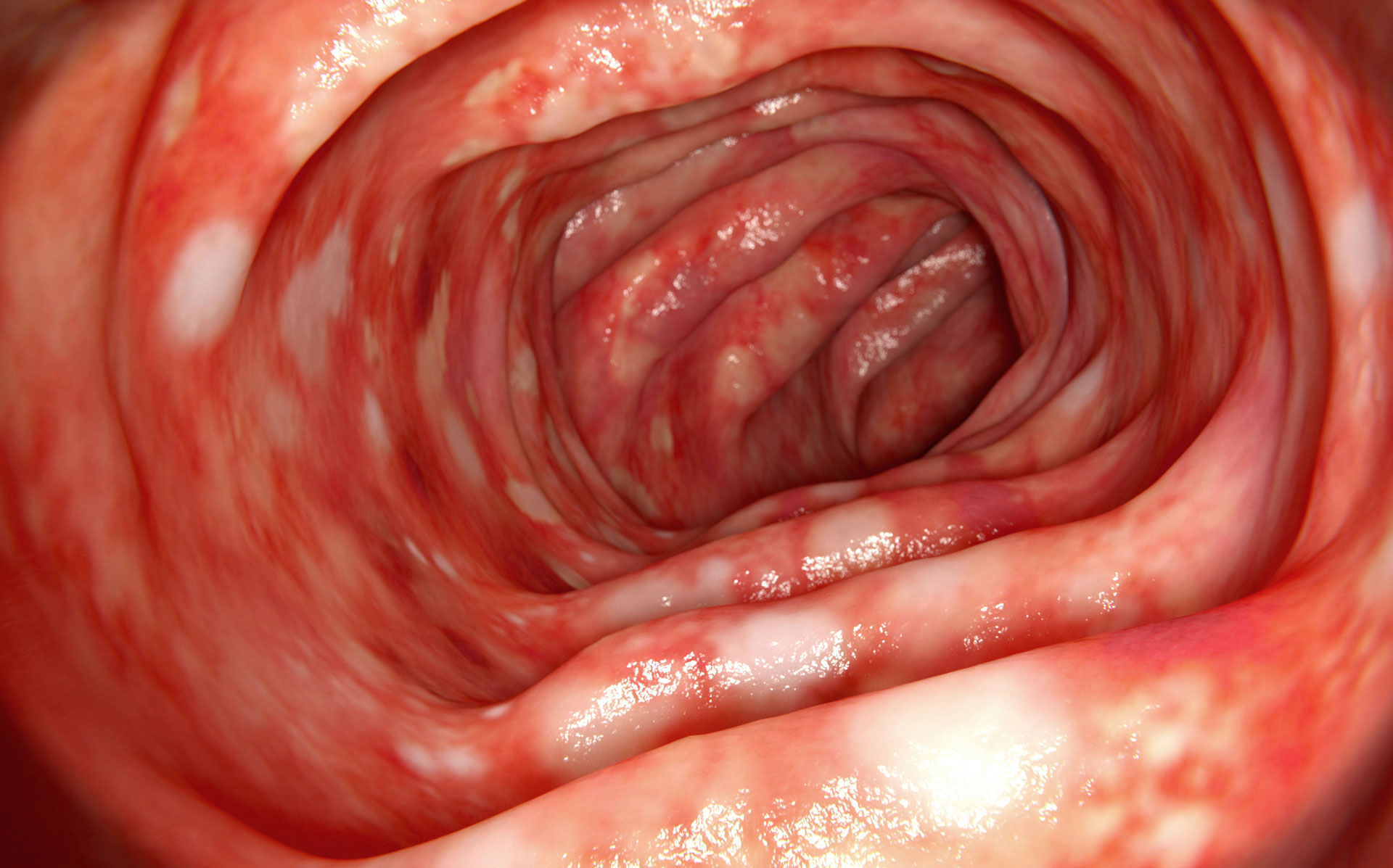
More than 300,000 people in Germany suffer from a progressive chronic inflammatory bowel disease (IBD), the most common forms being Crohn’s disease (approximately 300 cases per 100,000 people worldwide) and ulcerative colitis (250 to 500 cases per 100,000 people worldwide). Both conditions involve chronic inflammation of the gastrointestinal tract, which leads to symptoms such as abdominal pain or diarrhoea and potentially causes severe intestinal damage.
However, clinical signs like abdominal pain, cramps, diarrhoea, and/or flatulence can also be caused by infections, tumours, or non-inflammatory conditions such as irritable bowel syndrome (IBS). Without further diagnostic testing, it is often not possible to make a clear distinction.
Periods of flare-ups (relapses) with intensified symptoms alternate with phases of remission when the disease subsides. The duration and frequency of relapses vary significantly and cannot be predicted. Both types of IBD can also cause symptoms outside the digestive tract, affecting the skin, liver, eyes, joints, or bones. IBDs likely do not have a single cause but rather result from a multifactorial process: in addition to a possible genetic predisposition, other factors such as impaired intestinal barrier function (leaky gut), dysbiosis of the intestinal microbiota, intestinal infections, stress, and smoking often contribute to the onset or chronic progression of the disease.
Irritable Bowel Syndrome or Inflammatory Bowel Disease (IBD)?
Calprotectin is excreted in the stool during intestinal inflammation. Measuring faecal calprotectin reflects the extent of neutrophil migration into the intestinal lumen associated with IBD, with higher levels correlating with the severity of inflammation in the intestinal mucosa. Therefore, the detection of calprotectin in stool provides a simple, non-invasive method to clearly distinguish between non-inflammatory IBS symptoms and active intestinal inflammation, which is typically accompanied by morphological changes in the intestinal mucosa. However, calprotectin measurement does not indicate the specific underlying condition (e.g. Crohn’s disease versus ulcerative colitis); definitive diagnosis requires invasive imaging procedures. Nevertheless, calprotectin levels do correlate with endoscopic activity and histopathological grading in IBD, which makes it especially useful for reducing the need for endoscopy in paediatric patients.
Elevated EPX (eosinophil protein X) levels are also found in chronic inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis. Scientific studies have shown a clear correlation between inflammatory activity in Crohn’s disease and EPX levels in stool.
Calprotectin has high sensitivity in detecting chronic inflammatory bowel diseases, as well as polyps and colorectal carcinoma. Elevated calprotectin concentrations in stool can also occur in viral or bacterial infections of the gastrointestinal tract. Therefore, it is essential to first rule out infectious causes (e.g. via pathogen detection or pathogen-specific antibody testing) when clinically indicated, before initiating further diagnostic workup for suspected IBD.